WHA National Collaborative
"Women will be offered care that can reduce their chance of experiencing a tear"
Dr Barbara Vernon - Chief Executive Officer, Women's Healthcare Australasia
The National Collaborative drew on improvement methodologies developed by the US Institute for Healthcare Improvement(link is external) (IHI) in the US, and successfully employed by hospitals in the UK, the US and other places, to achieve sustained improvements in patient care. For some examples of the use of this methodology & its results overseas see: the Scottish Patient Safety Program.(link is external) The strength as a methodology is that it focuses on spread and adaptation of existing knowledge about best practice care to multiple settings to accomplish a common aim.
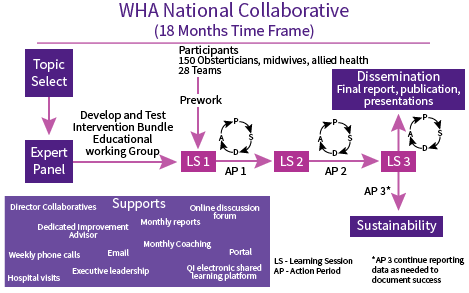
The Collaborative was hosted by Women’s Healthcare Australasia in partnership with the NSW Clinical Excellence Commission(link is external), supported by Safer Care Victoria (link is external)and the Clinical Excellence Division(link is external) of Queensland Health.
Teams signed up to participate in the WHA National Collaborative between September 2017 – December 2018 . They received extensive education, resources and regular improvement science coaching. Teams were supported to reliably implement the Perineal Protection Bundle© which included 5 elements of care known to reduce risk of harm from perineal tears.


